Lung Cancer: Symptoms, Types & Treatments
Understanding Lung Cancer
Lung cancer, a devastating disease impacting countless individuals worldwide, demands immediate attention and treatment. This article delves into the topic of lung cancer, exploring its causes, symptoms, diagnosis, and treatment options. By gaining a deeper understanding of this condition, individuals and their loved ones can make informed decisions about their health.
Exploring Lung Cancer Types and Symptoms
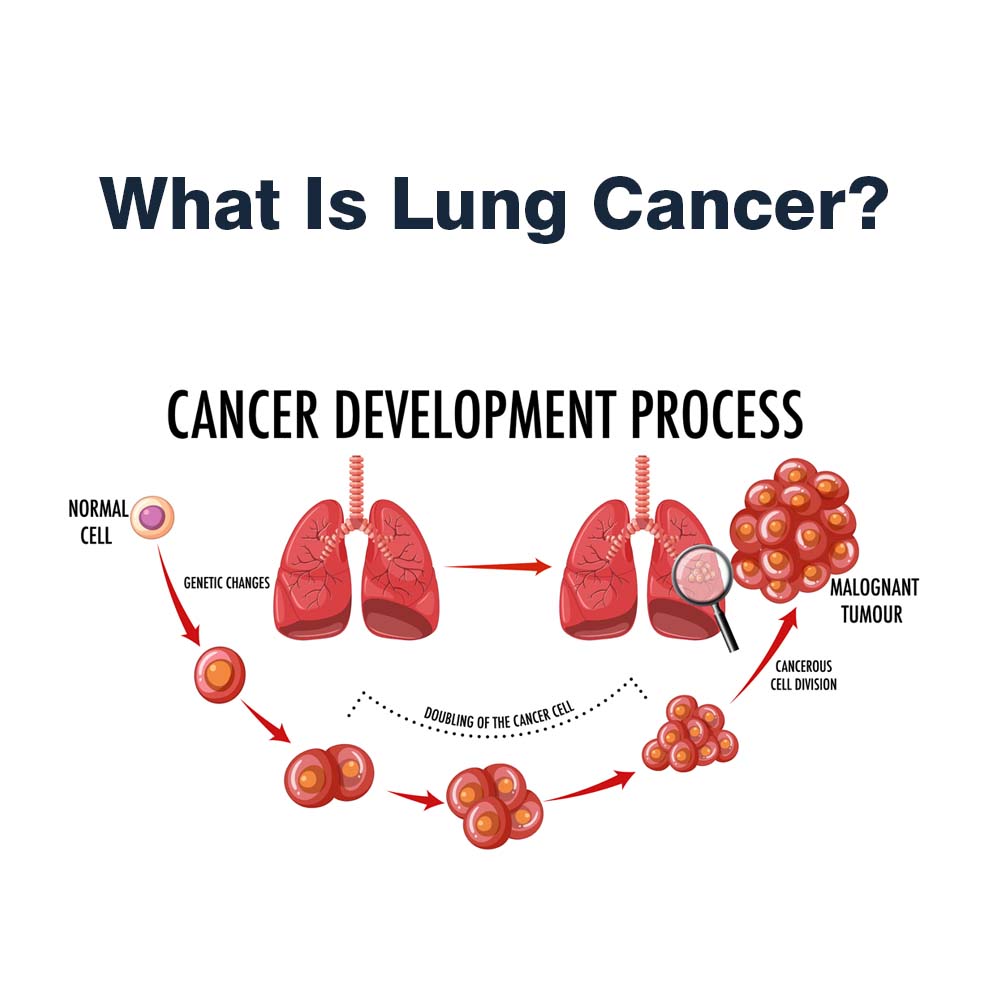
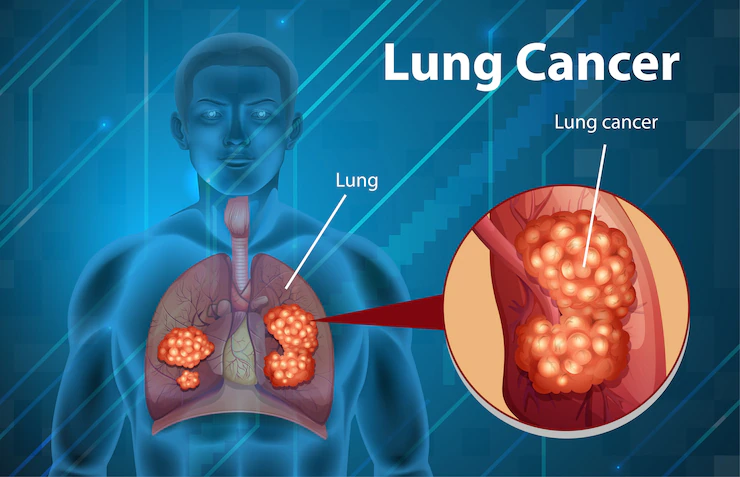
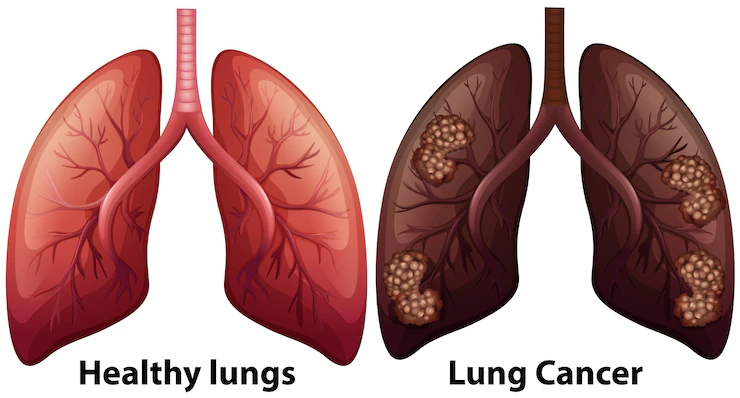
Lung cancer manifests through uncontrollable cell growth within the lungs and comprises two primary types: small-cell lung cancer and non-small-cell lung cancer. Further categorized into subtypes such as adenocarcinoma and squamous cell carcinoma, each type exhibits distinct growth patterns requiring specific treatment approaches.
The symptoms of lung cancer can vary, with some individuals experiencing respiratory-related issues, while others present symptoms connected to the spread of cancer to other body parts. Notably, many lung cancer cases remain asymptomatic until reaching an advanced stage.
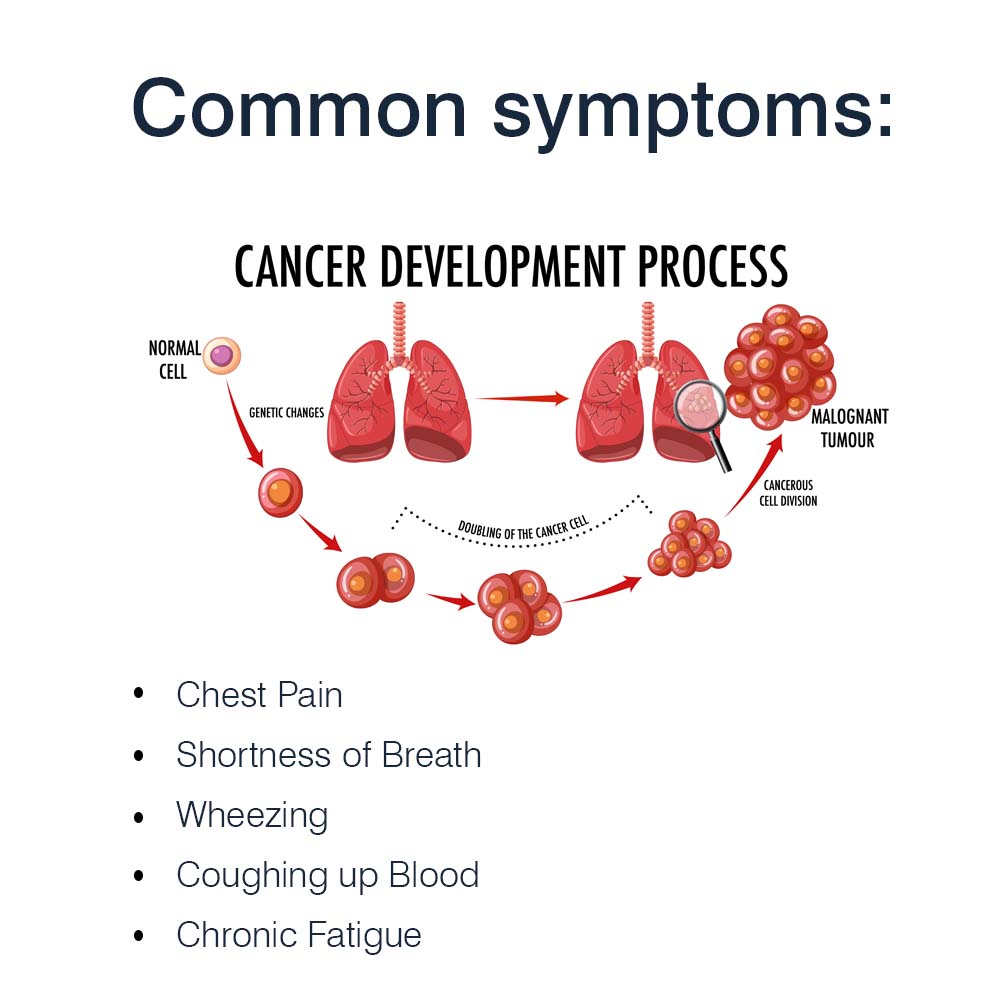
Common symptoms include:
- Persistent or Worsening Cough
- Chest Pain
- Shortness of Breath
- Wheezing
- Coughing up Blood
- Chronic Fatigue
- Unexplained Weight Loss
Additionally, lung cancer can cause other changes in the body, such as recurring pneumonia or the enlargement of lymph nodes in the chest area.
Other types of cancer in the lungs
Lung cancer can manifest in various types beyond the common lung cancer, including lymphomas (cancer in lymph nodes), sarcomas (cancer in bones or soft tissue), and pleural mesothelioma (cancer in the lining of the lungs). These types are treated differently and are not typically referred to as lung cancer.
The staging of lung cancer is based on factors like the size of the primary tumor, its extent into surrounding tissues, and whether it has spread to lymph nodes or other organs. Each type of cancer has its own staging guidelines.
For lung cancer, the general staging is as follows:
Stage 0 (in-situ): Cancer is present in the top lining of the lung or bronchus, without spreading to other lung parts or outside the lung itself.
Stage I: Cancer has not spread outside the lung.
Stage II: Cancer is larger than Stage I, has spread to nearby lymph nodes within the lung, or multiple tumors are present in the same lung lobe.
Stage III: Cancer is larger than Stage II, has spread to nearby lymph nodes or adjacent structures, or multiple tumors are found in a different lobe of the same lung.
Stage IV: Cancer has spread to the other lung, the fluid surrounding the lung, the fluid around the heart, or distant organs.
For small cell lung cancer (SCLC), it can be categorized as limited or extensive stage:
Limited stage SCLC is confined to one lung and may involve lymph nodes in the middle of the chest or above the collarbone on the same side.
Extensive stage SCLC has spread widely throughout one lung or to the other lung, lymph nodes on the opposite side of the lung, or other parts of the body.
These stages and classifications help medical professionals determine the appropriate treatment and prognosis for individuals with lung cancer.
Lung Cancer Treatment & Diagnosis
Facing suspected lung cancer necessitates a thorough diagnostic process to determine its stage and type. This process involves imaging tests, biopsies, and genetic mutation analysis.
Staging the cancer is vital for designing an appropriate treatment plan. Healthcare professionals tailor treatments to meet the unique needs of each individual by determining the extent of cancer's spread. Common treatment options for lung cancer include:
- Surgery: Surgical removal of cancerous tissue.
- Chemotherapy: Use of powerful drugs to destroy or shrink cancer cells.
- Radiation Therapy: Application of high-energy rays to eliminate cancer cells.
- Targeted Therapy: Use of specific drugs to inhibit the growth and spread of cancer cells.
Often, a multidisciplinary approach involving pulmonologists, surgeons, medical oncologists, and radiation oncologists is adopted to deliver the most effective treatment for each patient's condition.

Clinical Trials and Complementary Medicine
Clinical trials play a crucial role in advancing lung cancer treatment options, evaluating the safety and efficacy of new therapies. Individuals diagnosed with lung cancer are encouraged to explore participation in clinical trials to access potentially groundbreaking treatments.
Complementary and alternative medicine practices may also be considered alongside standard treatments. Complementary medicine includes practices like acupuncture, dietary supplements, massage therapy, hypnosis, and meditation, used in conjunction with conventional treatments.
Alternative medicine, on the other hand, involves non-traditional therapies replacing standard treatments, such as special diets, high-dose vitamins, herbal preparations, and magnet therapy. It is essential to consult with a healthcare professional before adopting any complementary or alternative medicine practices to assess their safety and potential benefits.
Choosing the Right Lung Cancer Treatment
Selecting the appropriate lung cancer treatment can be challenging. A specialized cancer doctor should be consulted, providing in-depth information about available treatment options based on the type and stage of cancer. These medical professionals can guide patients through the potential risks, benefits, and side effects associated with each treatment method. Seeking a second opinion from another reputable oncologist is also a viable option that can provide further clarity and peace of mind.
In Conclusion
Lung cancer is a complex disease demanding comprehensive understanding and proactive management. By familiarizing themselves with the causes, symptoms, diagnosis, and treatment options, individuals affected by lung cancer can take charge of their health journey. Early detection and timely intervention significantly improve the chances of successful treatment and long-term survival.