Cystic Fibrosis (CF): Symptoms, Causes, Diagnosis & Treatment
Cystic Fibrosis: The Facts You Need to Know
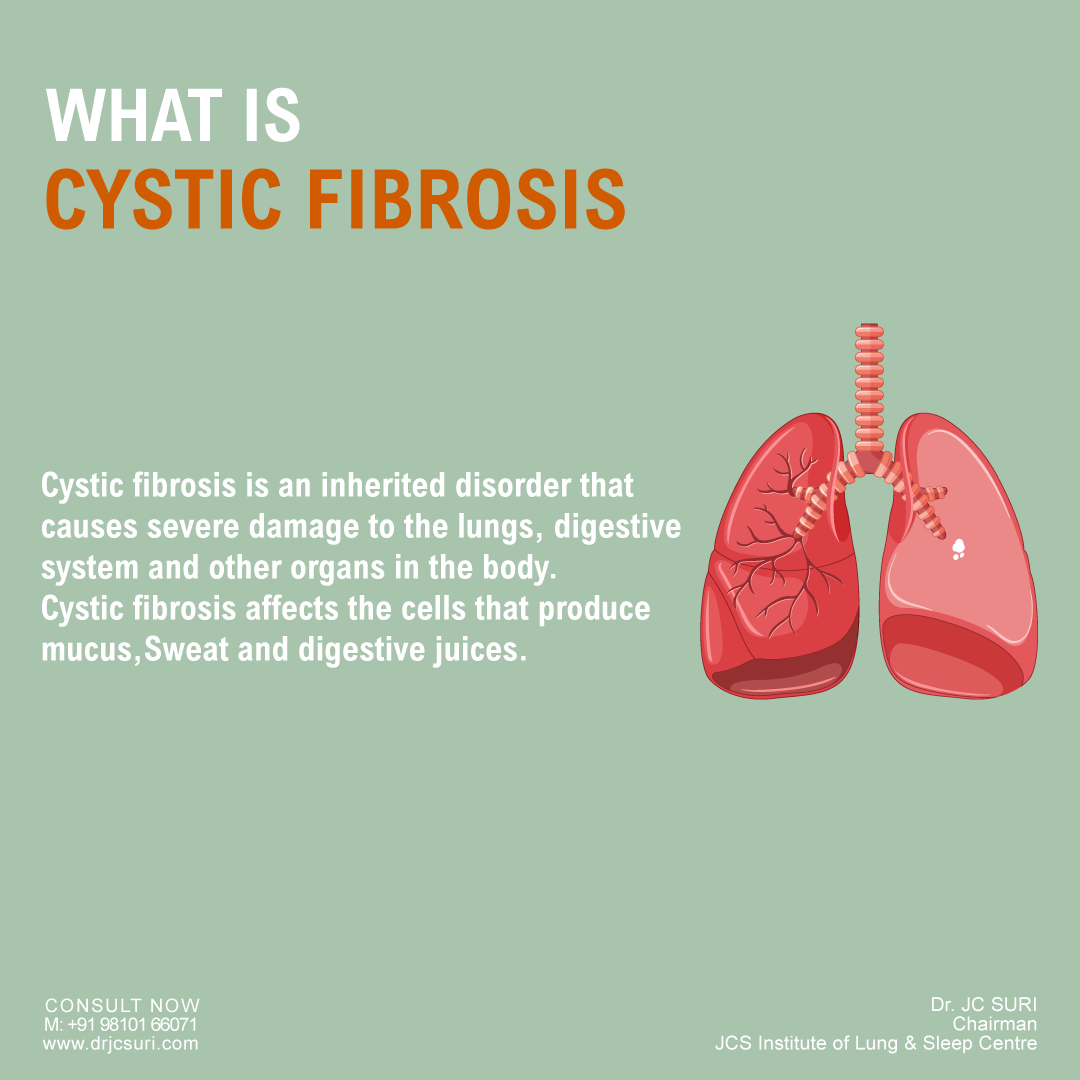
The lungs, digestive system, and other body organs are severely harmed by the genetic condition known as cystic fibrosis (CF).
Cystic fibrosis affects the cells that create mucus, sweat, and digestive secretions. These generated fluids are often thin and slippery. The secretions are thick and sticky in CF patients, though, due to a defective gene.
Particularly in the pancreas and lungs, the secretions obstruct the tubes, ducts, and channels instead of lubricating them.
Cystic fibrosis (CF) is a hereditary condition that you acquire from your parents at birth. It affects how your body makes mucus, a liquid that helps your organs and systems function.
When you have CF, your mucus is thick and glue-like rather than the normally thin and smooth consistency. Your body’s ducts and tubes become blocked as a result.
Additionally, it can result in serious lung damage such as fibrosis and cysts (fluid-filled sacs) (scar tissue). CF gained its name in this manner.
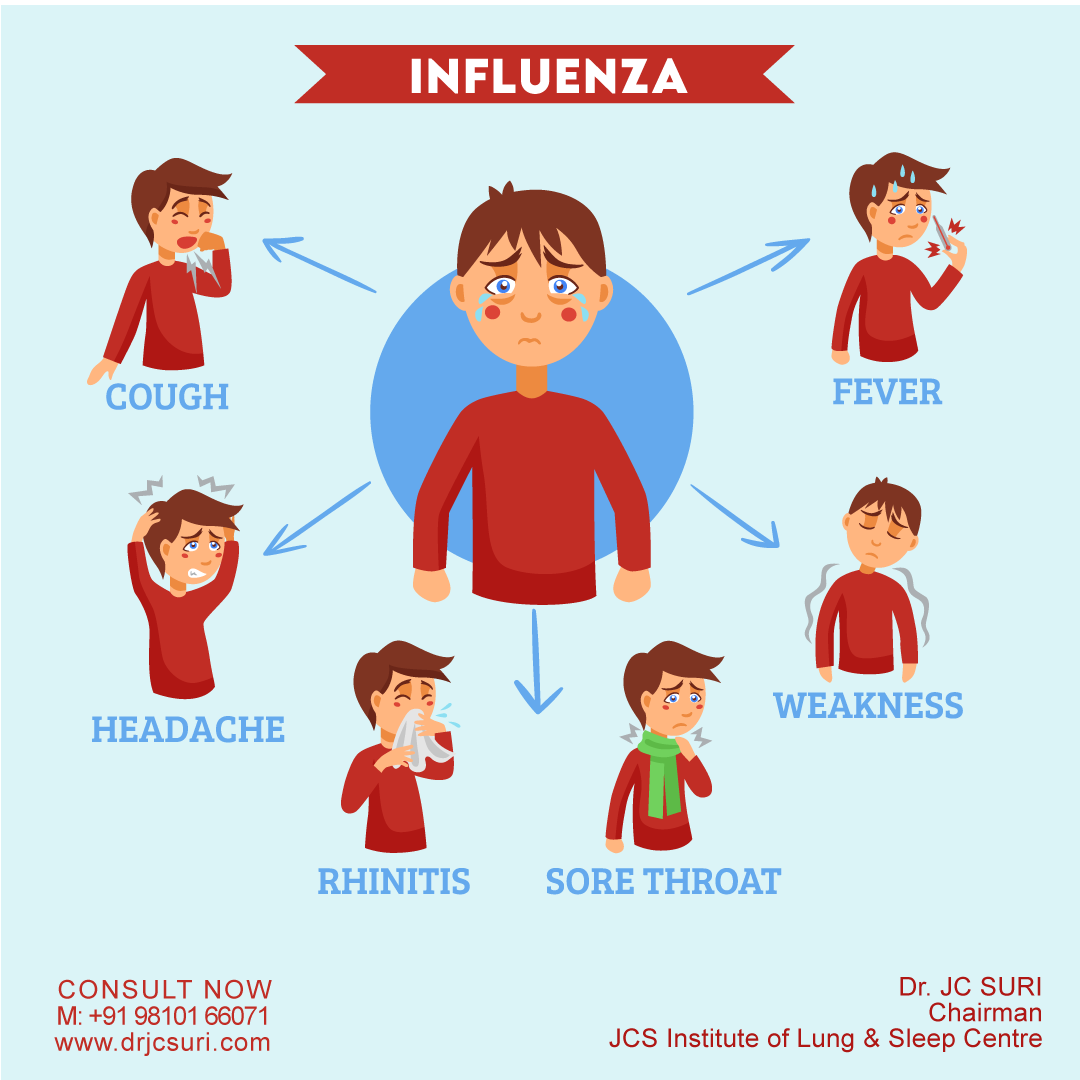
Cystic Fibrosis Symptoms
Depending on how severe the condition is, there are different suggestions and symptoms of cystic fibrosis. As time goes on, symptoms can get better or get worse, indeed in the same person.
Some people might not start showing symptoms until they’re teenagers or grown-ups. Adult cases are generally diagnosed with milder ails and are more prone to experience atypical symptoms, similar to intermittent pneumonia, infertility, and pancreatitis flare-ups.
- The trouble with bowel movements or frequent, slithery stools
- Gasping or having trouble breathing
- Frequent lung infections
- Infertility, especially in men
- Trouble growing or gaining weight
- Skin that tastes very salty
Cystic Fibrosis Causes
Cystic fibrosis is brought on by a mutation in the CFTR gene( cystic fibrosis transmembrane conductance regulator).
This gene regulates the movement of fluids and salt into and out of your cells. Sticky mucus accumulates in your body if the CFTR gene does not serve as it should.
You must inherit the gene with the mutation from both of your parents to develop CF. Ninety percent of persons who are affected have the F508del mutation in at least one copy.
If you have just one copy, you won’t show any signs of the illness, but you will be a carrier anyway. Therefore, there is a possibility that you will pass it on to your offspring.
Cystic Fibrosis Diagnosis
Early diagnosis means early treatment and better health later in life. Every state in the U.S. tests newborns for cystic fibrosis using one or more of these three tests:
Blood test- This test checks the levels of immunoreactive trypsinogen (IRT). People with CF have higher levels of it in their blood.
DNA test- This looks for mutations in the CFTR gene.
Sweat test- It measures the salt in your sweat. Higher than normal results suggest CF.
Cystic Fibrosis Treatment
There’s no cure for cystic fibrosis, but medications and other therapies can ease symptoms.
Medications- Your doctor may give you drugs to open your airways, thin mucus, prevent infections, and help your body get nutrients from food. These include:
Antibiotics- They can prevent or treat lung infections and help your lungs work better. You might get them as pills, in an inhaler, or a shot.
Anti-inflammatory medicines- These include ibuprofen and corticosteroids.
Bronchodilators- You’ll get these from an inhaler. They’ll relax and open your airways.
Mucus thinners- They’ll help you get the gunk out of your airways. You’ll get them from an inhaler.
CFTR modulators- These help CFTR work as it should. They can make your lungs work better and help you gain weight.
Combination therapy- The new medication elexacaftor/ivacaftor/tezacaftor (Trikafta) combines three CFTR modulators to target the CFTR protein and make it work efficiently.
Airway clearance techniques- These can help get rid of mucus. You might try:
Chest therapy or percussion- This involves tapping or clapping on your chest or back to clear mucus from your lungs. Someone else does this for you.
Oscillating devices- You inhale into a unique machine that vibrates or oscillates your airways. Mucus is loosened as a result, making coughing easier. An oscillating chest vest is an alternative.
Physical therapy for CF- This involves breathing techniques that force air through thick layers of mucus and against your chest wall. They facilitate clearing obstructed airways and make it simpler to cough up debris. Common exercises consist of:
Autogenic drainage- To accomplish this, you exhale forcefully, or huff. This facilitates the passage of mucus from your smaller to central airways and facilitates its removal.
Active cycle of breathing– This controls your breath and relaxes the upper chest and shoulders, which can help clear mucus and prevent airway blockages. You breathe in deeply, hold it, and then huff for different lengths of time.
Cystic Fibrosis Complications
The lungs aren’t the only part of your body CF damages. Cystic fibrosis also affects the following organs:
Pancreas- Your pancreas’ ducts are blocked by the thick mucus brought on by CF. This prevents digestive enzymes, which are proteins that help break down food, from getting to your intestine. Your body thus struggles to obtain the nutrition it requires. Diabetes may develop as a result of this over time.
Liver- Your liver becomes inflamed if the channels used to drain bile get blocked. This may result in cirrhosis, a severe scarring condition.
Small intestine- The lining of the small intestine can deteriorate because high-acid foods from your stomach can be challenging to digest.
Large intestine- The thick fluid in your stomach can make your poop large and harder to pass. This can lead to blockages. In some cases, your intestine may also start to fold in on itself like an accordion, a condition called intussusception.
Bladder- Chronic or long-lasting coughing weakens your bladder muscles. Almost 65% of women with CF have stress incontinence. This means that you leak a little pee when you cough, sneeze, laugh or lift something. Though it’s more common in women, men can have it, too.
Kidneys- Some people with CF get kidney stones. These small, hard globs of minerals can cause nausea, vomiting, and pain. If you don’t treat them, you could get a kidney infection.
Reproductive organs- Both male and female fertility is impacted by excess mucus. Most CF sufferers have issues with the vasa deferentia, which transport sperm. Due to their extremely thick cervical mucus, women with CF may have trouble getting sperm to fertilize eggs.
Other parts of the body- Additionally, osteoporosis and muscle weakness are side effects of CF. Low blood pressure, weariness, a rapid heartbeat, and a general sensation of weakness can also result from it because it throws off the balance of minerals in your blood.
Read more “Cystic Fibrosis (CF): Symptoms, Causes, Diagnosis & Treatment”