Sarcoidosis: Causes, Symptoms, Diagnosis & Treatment
Sarcoidosis, a rare disease that triggers the formation of lumps or nodules known as granulomas, can affect various parts of the body, including the lungs, lymph nodes, skin, and eyes. This enigmatic condition, characterized by its diverse range of symptoms, demands a deeper understanding to navigate its complexities effectively.
What is Sarcoidosis?
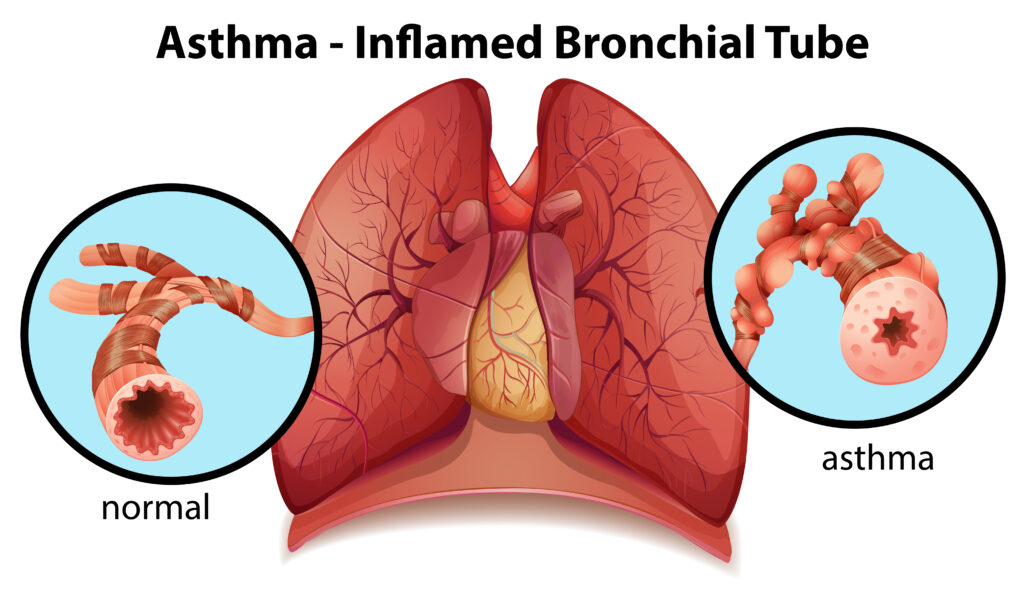
Sarcoidosis manifests when the immune system goes into overdrive, creating granulomas. These granulomas, comprised of clustered white blood cells, can vary in size and location, leading to a spectrum of symptoms. From mild discomfort to severe manifestations, these granulomas are a hallmark of sarcoidosis. In some cases, they progress into fibrosis, resulting in permanent lung scarring.
The Anatomy of Granulomas:
Granulomas, the focal points of inflammation, consist of white blood cells enclosed within dense fibrous tissue. This encapsulation forms hard and lumpy nodules, contributing to the distinct characteristics of sarcoidosis. The body initiates this process to shield itself from perceived threats, demonstrating the intricate mechanisms of the immune system in action.
Affected Areas:
While granulomas can develop anywhere in the body, they predominantly affect the lungs and lymph nodes. Additionally, these inflammatory clusters may manifest visibly in the skin, eyes, or muscles, leading to specific and recognizable symptoms for accurate diagnosis and management.
Demographic Insights:
Sarcoidosis does not discriminate but shows a predilection for certain demographics. It is more prevalent in the Black population than in whites, and it affects individuals assigned female at birth slightly more than those assigned male at birth. Typically, sarcoidosis emerges between the ages of 25 and 40, painting a demographic picture that aids in early detection and targeted interventions.
Genetic Predisposition:
While sarcoidosis is not directly hereditary, individuals with first-degree biological relatives diagnosed with the condition face a higher risk. Genetic factors, intertwined with environmental triggers, underscore the importance of understanding one’s family medical history for proactive health management.
Prevalence and Rarity:
Sarcoidosis, by definition, is a rare disease, with fewer than 200,000 reported cases in the U.S. at any given time. Despite its rarity, the condition necessitates heightened awareness, comprehensive research, and support for affected individuals to improve diagnostic accuracy and develop effective treatment strategies.
Symptoms and Causes
What are the symptoms of sarcoidosis?
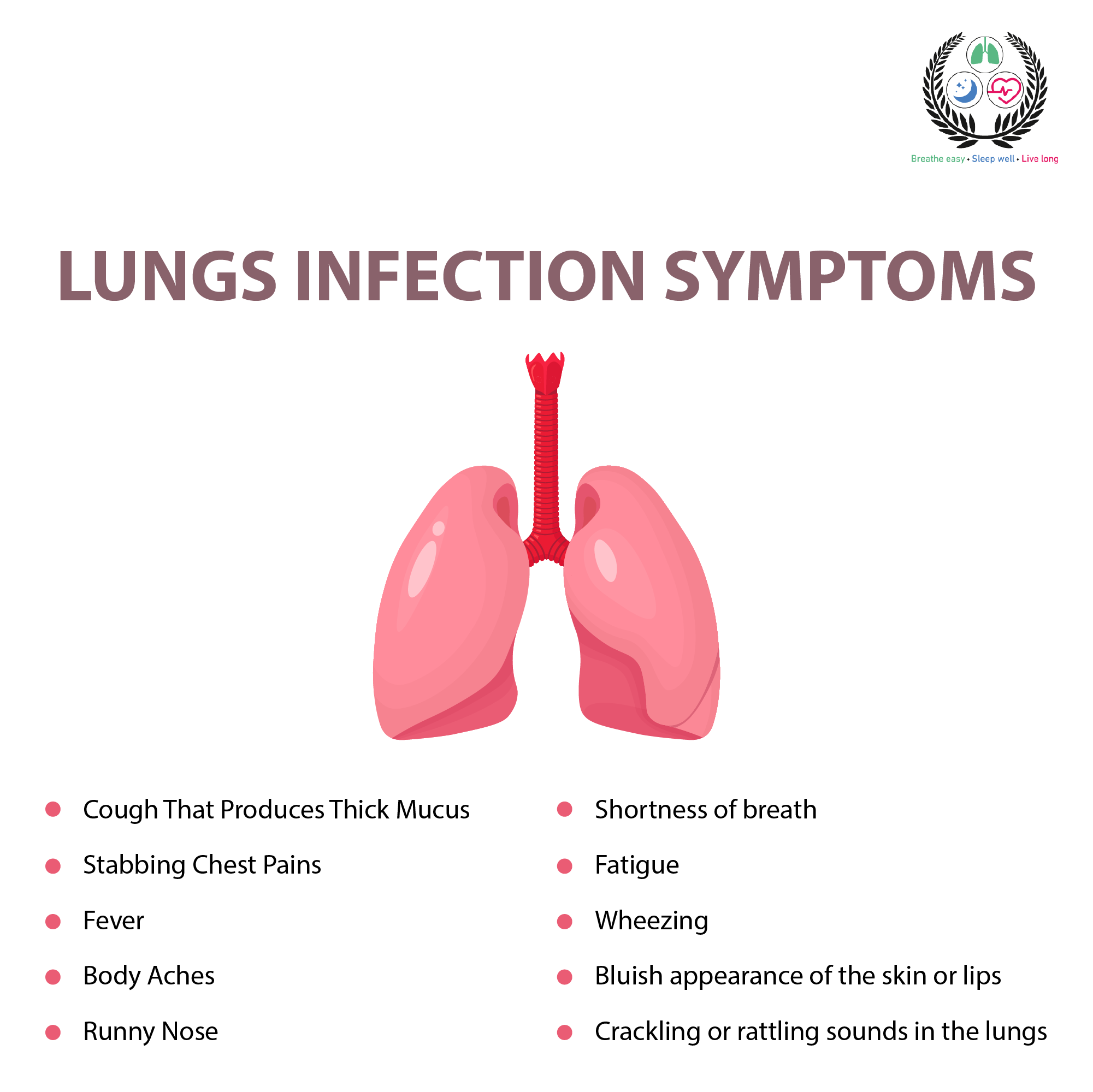
The symptoms of sarcoidosis depend on where in your body granulomas form. Most people with sarcoidosis have lung symptoms, but you can have symptoms in your skin, eyes, joints and almost anywhere else in your body. You may also have general feelings of being unwell or no symptoms at all.
General symptoms of sarcoidosis:
Fever
Fatigue
Joint pain
Muscle aches or weakness
Night sweats
Swollen lymph nodes
Unexplained weight loss
Kidney stones
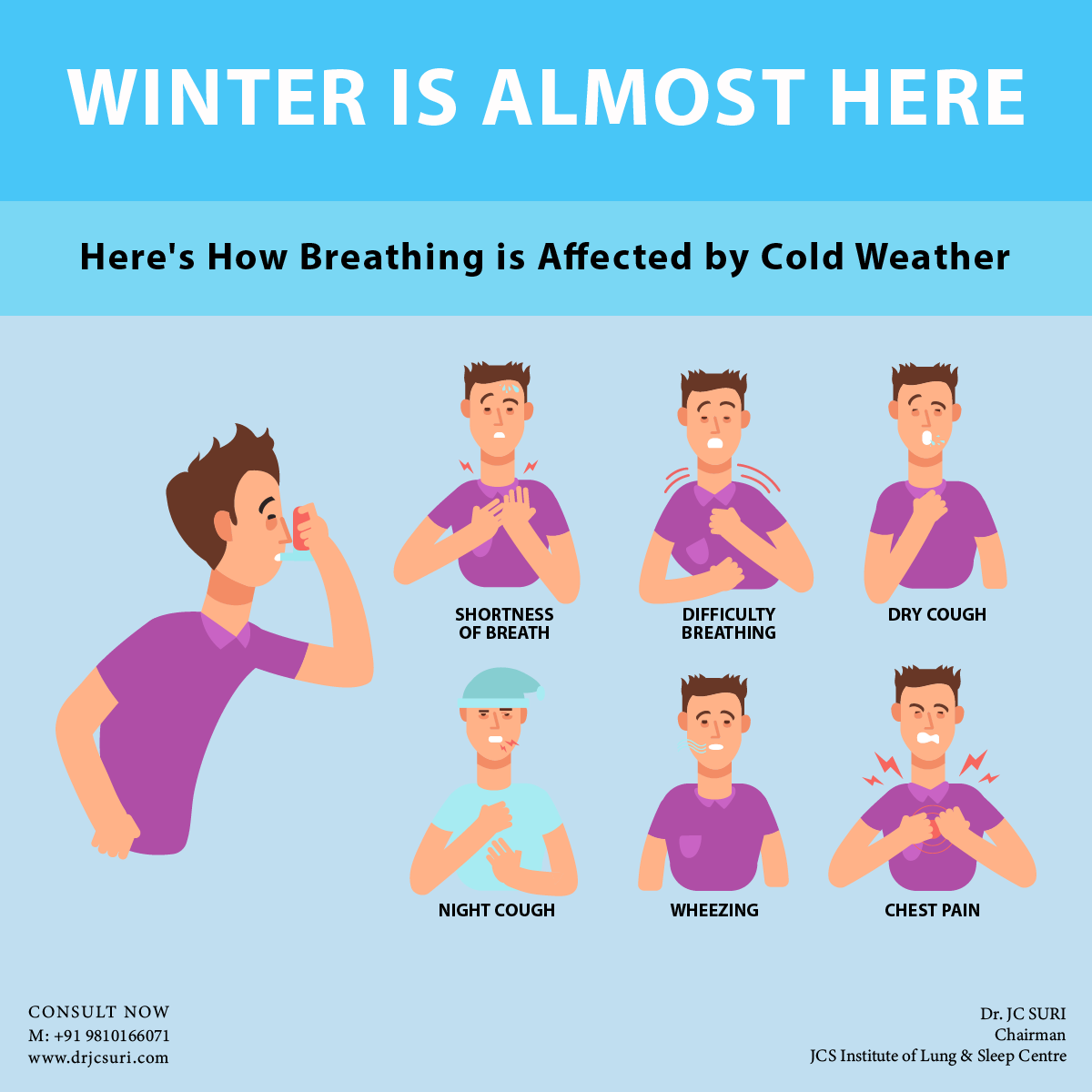
Symptoms of sarcoidosis in your lungs:
Cough
Shortness of breath (dyspnea)
Chest pain
Wheezing
Symptoms of sarcoidosis in your eye:
Blurred vision or loss of vision (optic neuritis)
Eye pain
Red or swollen eyes (uveitis or conjunctivitis)
Sensitivity to light
Symptoms of sarcoidosis of your skin:
Growths under your skin around scars or tattoos
Light or dark patches of skin
Raised, reddish-purple sores or rash across your nose or cheeks (lupus pernio)
Red, tender bumps on your shins (erythema nodosum)
Symptoms of sarcoidosis of your heart:
Chest pain
Fluttering heartbeat (palpitations)
Irregular heartbeat (arrhythmia)
Heart failure
Shortness of breath
Symptoms of sarcoidosis of your nervous system:
Increased thirst or amounts of pee (Diabetes insipidus)
Weak or paralyzed facial muscles (Bell’s palsy)
Headaches
Seizures
Pulmonary sarcoidosis, a condition affecting the lungs, is often categorized into stages using the Siltzbach classification system. It’s essential to note that these stages do not necessarily indicate the severity of the condition, and individuals may not progress through each stage.
Instead, they are primarily based on the appearance of the lungs in chest X-rays and describe the locations of granulomas within the lungs and lymph nodes.
Stage 0: In this stage, chest X-rays do not reveal any signs of pulmonary sarcoidosis. Both the lungs and lymph nodes appear normal, providing no evidence of the condition’s presence.
Stage 1: Stage 1 involves the presence of granulomas exclusively within the lymph nodes. While these granulomas are present, they do not yet affect the lungs themselves.
Stage 2: At this stage, granulomas can be observed in both the lymph nodes and the lungs. This marks a progression from Stage 1, with the condition now impacting both areas.
Stage 3: In Stage 3, granulomas are found solely within the lungs. This stage signifies that the condition has become more localized and primarily affects the pulmonary region.
Stage 4: The final and irreversible stage is Stage 4. At this point, X-rays reveal pulmonary fibrosis, which denotes permanent scarring of the lungs. This stage represents a significant change in the condition’s nature, as it leads to lasting lung damage.
It’s important to understand that pulmonary sarcoidosis is dynamic, and individuals may move between these stages or experience the complete disappearance of granulomas. However, Stage 4 is the exception, as it indicates permanent and irreversible lung scarring.
What causes sarcoidosis?
Research suggests that sarcoidosis stems from a complex interplay of genetic predisposition and environmental factors, although its precise cause remains elusive. Studies suggest that certain individuals are more susceptible to an exaggerated immune response triggered by specific antigens, such as bacteria and viruses.
While the immune system is intricately involved, it’s crucial to note that sarcoidosis is not classified as an autoimmune disorder. The exact mechanisms underlying this condition continue to be a subject of ongoing scientific exploration and inquiry.
Since we don’t know for sure which combination of genes and triggers causes sarcoidosis, it’s impossible to predict who will get it.
Diagnosis & Treatment
How is sarcoidosis diagnosed?
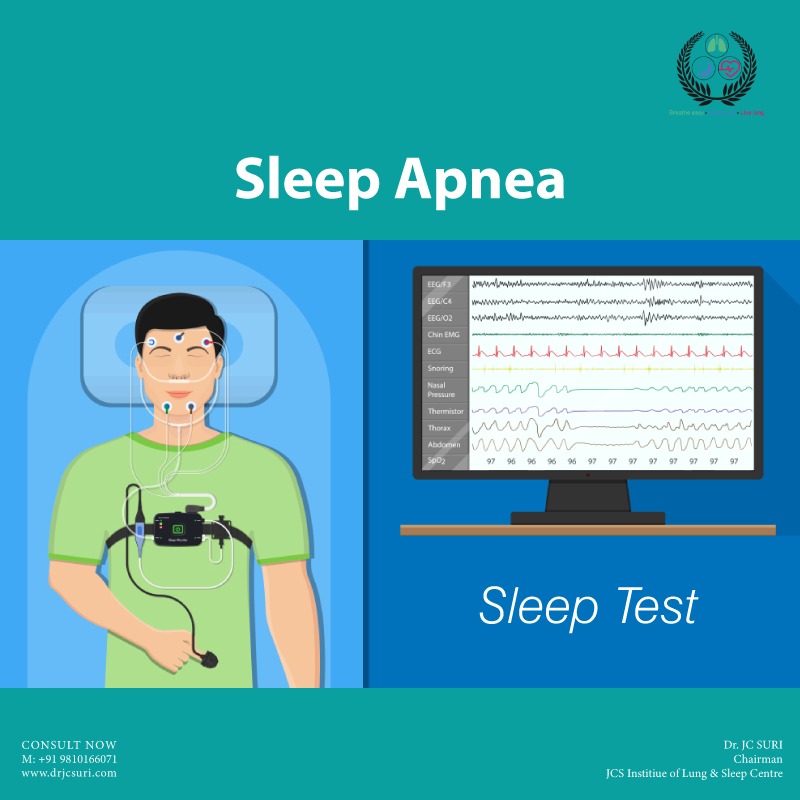
Sarcoidosis diagnosis typically involves a physical exam, imaging like chest X-rays, and biopsy of suspected granulomas. Additional tests might be conducted to rule out similar conditions due to sarcoidosis’s resemblance to other illnesses.
How is sarcoidosis treated?
Sarcoidosis treatment focuses on symptom management and preventing organ damage. Medications that modify or suppress the immune system are commonly prescribed, tailored to the location of granulomas in the body. While there’s no specific cure, sarcoidosis often resolves spontaneously, and if symptoms are mild or non-life-threatening, immediate treatment might not be necessary. Patients work closely with healthcare providers to monitor symptoms and determine the most suitable course of action.
Complications/side effects of treatment
Corticosteroids can put you at increased risk of getting sick with an infectious disease and can cause a number of side effects, including:
Excessive weight gain
Insomnia
Acne
Diabetes in susceptible people
High blood pressure
Glaucoma
Cataracts
Osteoporosis
Depression and emotional irritability
Skin bruising
For this reason, healthcare providers only recommend using medications to treat sarcoidosis if the benefits outweigh the risks.
Prevention
How can I prevent sarcoidosis?
The cause of sarcoidosis prevention strategies remain elusive. However, adhering to prescribed medications under healthcare provider guidance can significantly decrease the risk of organ damage caused by granulomas. While the origins of sarcoidosis remain uncertain, proactive management is key to mitigating its potential impact.